Muscle tension dysphonia is one of the most common voice disorders in adults, and paradoxically one of the most difficult for patients to understand. The voice deteriorates, becomes tired, unstable, or uncomfortable, even though medical examinations often provide reassurance.
This page aims to clarify what muscle tension dysphonia really is, what medical and speech therapy treatment can achieve, and in which cases functional voice coaching can effectively complement this work
What is muscle tension dysphonia?
Muscle tension dysphonia (MTD) is afunctional voice disorder. It is not related to damage to the vocal cords, but to overactivation or poor coordination of the muscles involved in phonation.
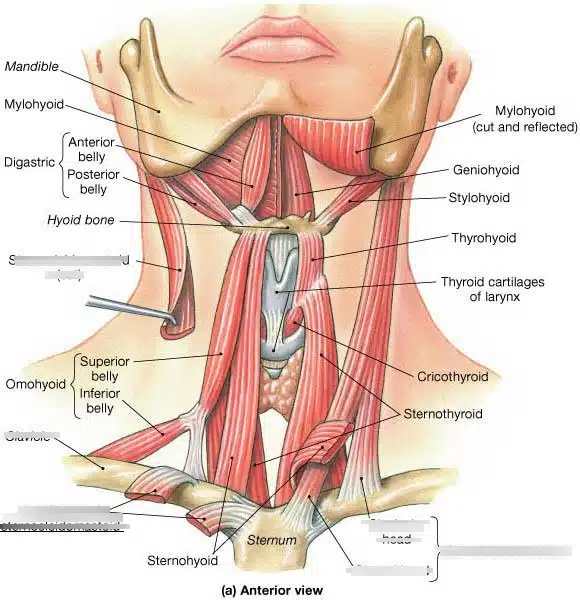
In concrete terms, the muscles of the larynx, as well as those surrounding it (jaw, tongue, neck, shoulders), work excessively or inappropriately. This hyperactivity disrupts the normal balance between breathing, vocal cord vibration, and resonance.
The voice then becomes difficult to produce, unstable, and sometimes painful, without any clear anatomical damage being observable during examinations.
Common symptoms of muscle tension dysphonia
Altered voice quality
- Hoarse, tight, or strained voice
- Breathy or unstable voice
- Difficulty projecting effortlessly
- Loss of flexibility and modulation
Fatigue and discomfort
- Rapid vocal fatigue
- Feeling of constant effort when speaking
- Tension in the throat, jaw, neck, or shoulders
- Less reliable voice at the end of the day or under stress
Key point: these symptoms often persist despite normal ENT examinations, which can lead to misunderstanding and discouragement.
Why does this dysphonia develop?
Muscle tension dysphonia is rarely linked to a single cause. It is most often the result of a combination of factors that add up and become self-perpetuating.
Functional factors
- Intensive or prolonged vocal use
- Inappropriate vocal technique
- High or inefficient breathing
- Constrained posture
Emotional and contextual factors
- Chronic stress
- Professional or social pressure
- Need to be heard in noisy environments
In many cases, tension initially appears as a compensatory strategy. Over time, this strategy becomes the default mode of voice functioning.
The central role of medical and speech therapy diagnosis
A fundamental point: any persistent dysphonia must be medically evaluated. The role of the ENT specialist or phoniatrist is to rule out any organic pathology and to assess the condition of the vocal cords.
The speech therapist then steps in to:
- analyze vocal production
- correct respiratory imbalances
- reduce laryngeal tension
- restore healthy phonation
This work is essential and forms the basis of any healthy vocal recovery.
Why the voice may remain unstable despite speech therapy
In some people, the condition has stabilized and speech therapy has been completed, but the voice remains fragile in real life: persistent fatigue, recurring tension, difficulty speaking for long periods or in demanding contexts.
This discrepancy can often be explained by:
- deeply ingrained compensatory patterns
- insufficient use of the extralaryngeal muscles
- a lack of transfer to complex vocal situations (stress, speaking, projection)
The role of functional vocal coaching
The vocal support offered here is strictly non-medical. It does not provide diagnoses, does not treat pathologies, and never replaces speech therapy.
It works as a complement, once a medical framework has been established, to address the real, everyday use of the voice.
Work on extralaryngeal musculature
Muscle tension dysphonia very often involves tension in the jaw, tongue, floor of the mouth, cervical area, and shoulders. These areas directly influence laryngeal freedom.
Vocal coaching aims to identify and release these locking points in order to restore more efficient and economical phonation.
Breath–phonation–resonance coordination
Beyond the mere absence of pain, the goal is to improve overall vocal coordination: respiratory support, efficient vibration, and optimal resonance, without strain.
This work leads to a voice that is more stable, more comfortable, and better tolerated over time.
Who is this support suitable for?
- Persistent vocal fatigue despite speech therapy follow-up
- Medically stabilized muscle tension dysphonia
- Intensive professional use of the voice
- A need for daily vocal reliability and comfort
A complementary approach, respectful of medical care
Muscle tension dysphonia is not a matter of opposition between medical treatment and functional support. On the contrary, it requires clear collaboration between medicine, speech therapy, and functional voice work.
The objective is not merely to have a “normal” voice during an examination, but a voice that is usable, comfortable, and reliable in real life.
Summary: Do you feel that your voice “wears out” before the end of the day? Vocal fatigue and muscle tension are not inevitable. Learn how to identify inefficient vocal habits and how vocal coaching helps release your communication.

